Transforming Medicine
|
Until recently, visualizing the architectural and cellular morphology of human tissue has required histopathological examination. Samples would be excised from the patient, processed, sectioned, stained and viewed under a microscope. In addition to being invasive, time consuming, and costly, the static nature of conventional pathology prohibits the study of biological dynamics and function. The Tearney Laboratory at Massachusetts General Hospital leads the way in transforming the current diagnostic paradigm through the invention and translation of new noninvasive, high-resolution optical imaging modalities that enable disease diagnosis from living patients without excising tissues from the body.
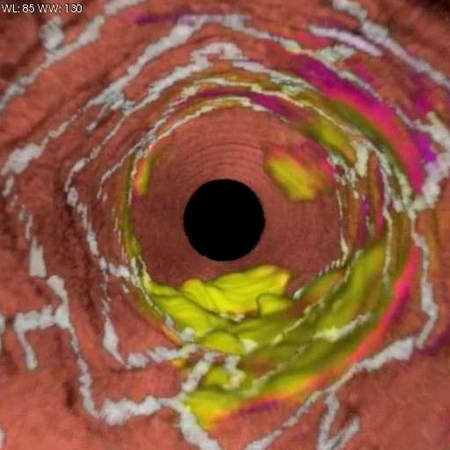
Led by Guillermo (Gary) Tearney, MD, PhD, the lab’s large multidisciplinary team invents, validates and translates novel devices that use light to conduct microscopy in living patients. Light is uniquely well suited for noninvasively interrogating the microscopic structure, molecular composition and biomechanical properties of biological tissues. The goal of the laboratory’s research is to improve understanding and diagnosis of disease by imaging the human body at the highest possible level of detail in vivo. Coronary artery imaged with
|
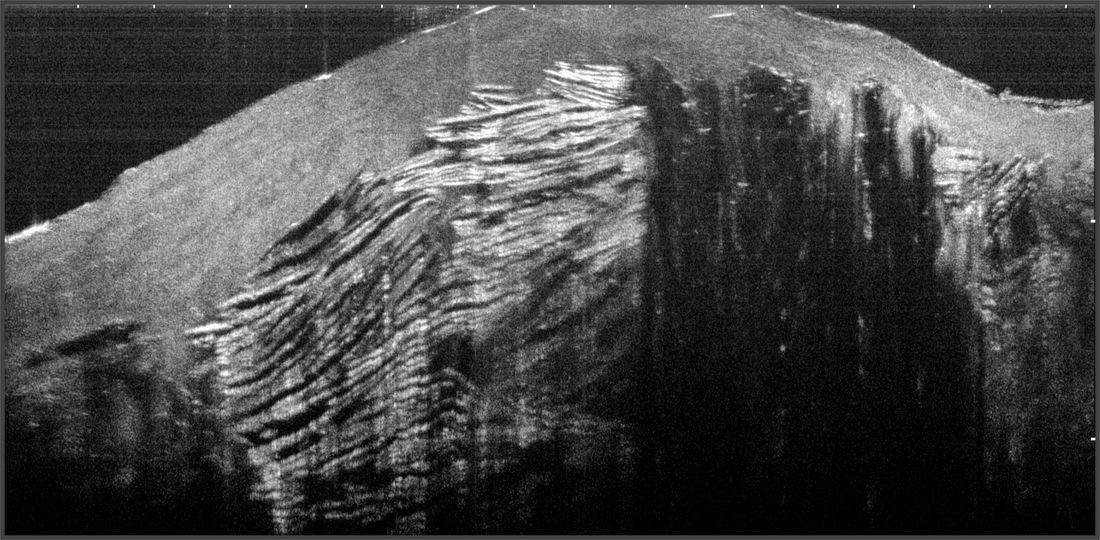
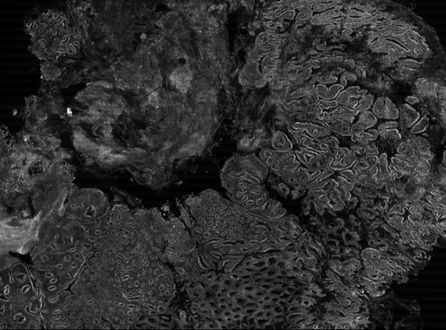
Dysplastic Barrett's Esophagus imaged with SECMThe stomach imaged with OCT CapsuleCilia lining the trachea imaged with µOCTAmpulla of Vater imaged with OCT Capsule |
The Tearney Lab's Swallowable Capsule is named one of MIT Technology Review's
Top 10 Breakthrough Technologies for 2019
Photo Credit - Bruce Peterson
We are thrilled that this year's guest curator, Bill Gates, chose our capsule to be included in MIT Technology Review's Top 10 Breakthrough Technologies!
"The little probe will help researchers answer questions about EED’s (Environmental enteric dysfunction) development—such as which cells it affects and whether bacteria are involved—and evaluate interventions and potential treatments". —Courtney Humphries
You can read more about this here
"The little probe will help researchers answer questions about EED’s (Environmental enteric dysfunction) development—such as which cells it affects and whether bacteria are involved—and evaluate interventions and potential treatments". —Courtney Humphries
You can read more about this here
Dr. Tearney's journey as a Mass General Research Scholar is featured in the Summer 2018 issue of Mass General Magazine
“The MGH Research Scholars program offers greater freedom,” says Dr. Tearney, who was the Mike and Sue Hazard Family MGH Research Scholar from 2012 to 2017. “You can have a crazy idea that nobody believes will work, and you can try it.”
“The funding allowed me to generate completely new projects that resulted in preliminary data that ended up getting new grants from the National Institutes of Health (NIH),” he continues. “Those grants wouldn’t have happened if I hadn’t had the freedom to try those high-risk ideas that the MGH Research Scholars program allowed me to pursue.”
“The funding allowed me to generate completely new projects that resulted in preliminary data that ended up getting new grants from the National Institutes of Health (NIH),” he continues. “Those grants wouldn’t have happened if I hadn’t had the freedom to try those high-risk ideas that the MGH Research Scholars program allowed me to pursue.”
| |||||||
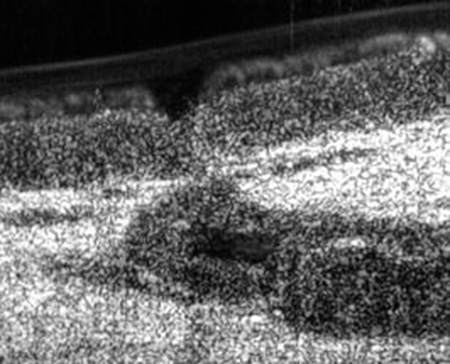
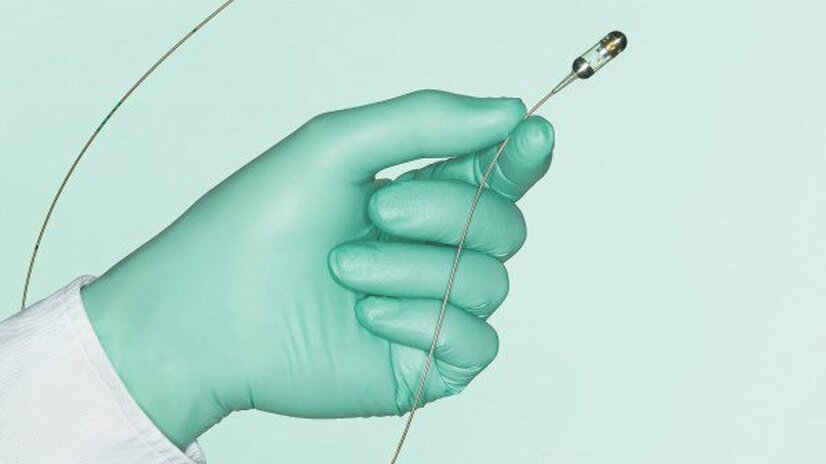
Implantable microscopes
for seeing cells in living tissue continuously
The Tearney Lab is developing implantable microscopes that can be implanted directly into the body to monitor cells as they move and interact. This long-term, high-resolution view of cells will transform our understanding of disease and how to treat it.
Wireless Implantable Microscope (WIM)
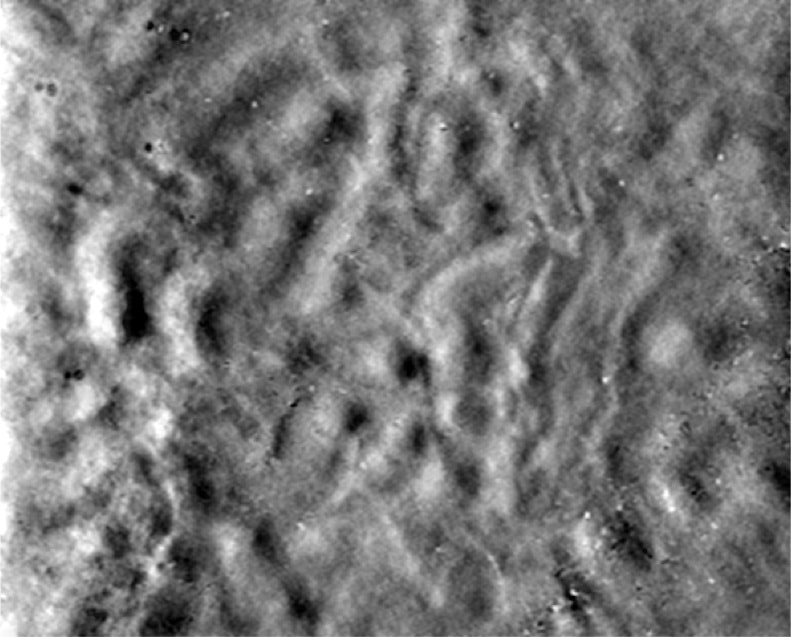
Renal tubule cells imaged 24 hours after WIM implantation